SHM Submits Comments on Proposed MACRA QPP
August 21, 2017
SHM's Policy Efforts
SHM supports legislation that affects hospital medicine and general healthcare, advocating for hospitalists and the patients they serve.
Download Letter
Centers for Medicare & Medicaid Services
Department of Health and Human Services
Attention: CMS-5522-P
P.O. Box 8013
Baltimore, MD 21244-8013
Dear Administrator Verma:
The Society of Hospital Medicine (SHM), on behalf of the nation’s nearly 57,000 hospitalists, appreciates the opportunity to provide comments on the proposed rule CMS-5522-P Medicare Program; CY 2018 Updates to the Quality Payment Program. In this proposed rule, CMS further develops the Quality Payment Program and its two pathways for provider payment: the Merit-based Incentive Payment System (MIPS) and Alternative Payment Models (APMs).
Hospitalists are front-line healthcare providers in America’s hospitals for millions of hospitalized patients each year, many of whom are Medicare and Medicaid beneficiaries. As leaders of an interdisciplinary care team, they manage the inpatient medical needs of their patients, while working to enhance the performance of their hospitals and health systems. Although most hospitalists are Board Certified in Internal Medicine or Family Medicine, they practice exclusively in facility settings and do not have outpatient office practices. Hospital medicine practitioners have a variety of employment structures, ranging from direct employment by a hospital or health system to independent staffing groups that contract with a hospital.
The position of hospitalists within the healthcare system affords a distinctive role in facilitating both the individual physician-level and systems or hospital-level performance agenda. This includes participation and performance assessment in programs around value-based purchasing and quality improvement.
Broadly, SHM is supportive of many of the proposed policies in the Quality Payment Program (QPP) proposed rule. It continues some of the reporting and scoring flexibilities promulgated in the 2017 QPP rule which are helpful as providers continue to learn about the program requirements and develop reporting processes. CMS also proposes to implement a facility-based measurement option, which would enable hospitalists and other facility-based providers to align their MIPS scores with their institutions.
We offer comments below on specific proposals in the rule:
Merit-based Incentive Payment System (MIPS)
II.C.6.b.3 Quality Data Submission Criteria
CMS proposes to maintain the required number of measures for the MIPS Quality category at six (6) for the 2018 performance year. While we appreciate that CMS has maintained the six measures requirement rather than increasing this number, we remind CMS that even six measures may be a challenge for some providers, including hospitalists, to meet. Concerted efforts should be made to ensure that those providers who have fewer than six measures available for reporting are not disadvantaged in any way.
As is noted in the rule, if fewer than six measures apply to an individual MIPS eligible clinician or group, they would need to report on each measure that is applicable. CMS would make determinations on whether a sufficient number of measures were applicable and reported for those providers who report by the claims and registry mechanisms. In mid-2017, CMS outlined processes for the Eligible Measure Applicability (EMA), which would check whether providers reported on a sufficient number of applicable measures. We strongly encourage CMS to make this process as transparent as possible by publishing additional guidance and information about the EMA. Due to the relatively few number of measures available to them, hospitalists will need to rely on the EMA to ensure they are not receiving unnecessary zeroes in numerators for unreported measures in the Quality Category.
CMS also makes a proposal that an individual MIPS eligible clinician or group can report on a specialty measure set and, if the specialty measure set has fewer than six measures, report all available measures in the set. We support the amended specialty measure set for hospitalists (Table Group B.27. Hospitalists) that contains six measures. These are the only consistently-reportable measures for hospitalists in the MIPS measure inventory.
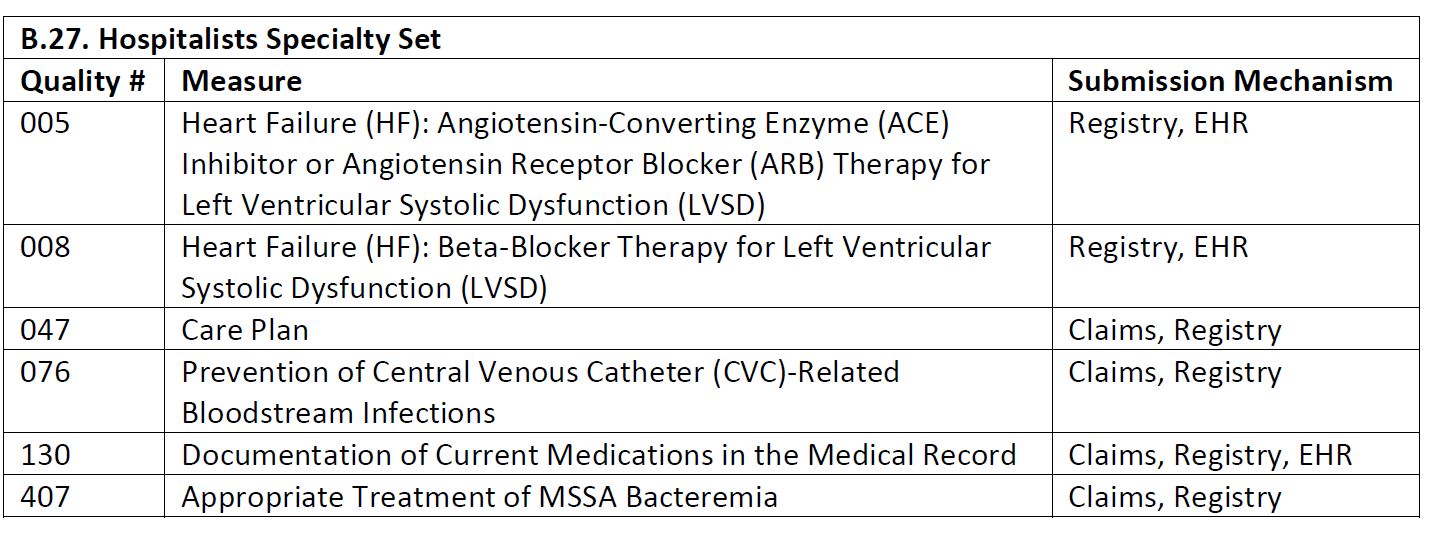
As Table B.27 indicates, hospitalists can only report on four measures (47, 76, 130, 407) for claims-based reporting. For registry reporting, hospitalists could report on all six measures. We note that because of the nature of their practice, hospitalists generally cannot use the EHR reporting mechanism, as they are using their hospitals’ EHR systems.
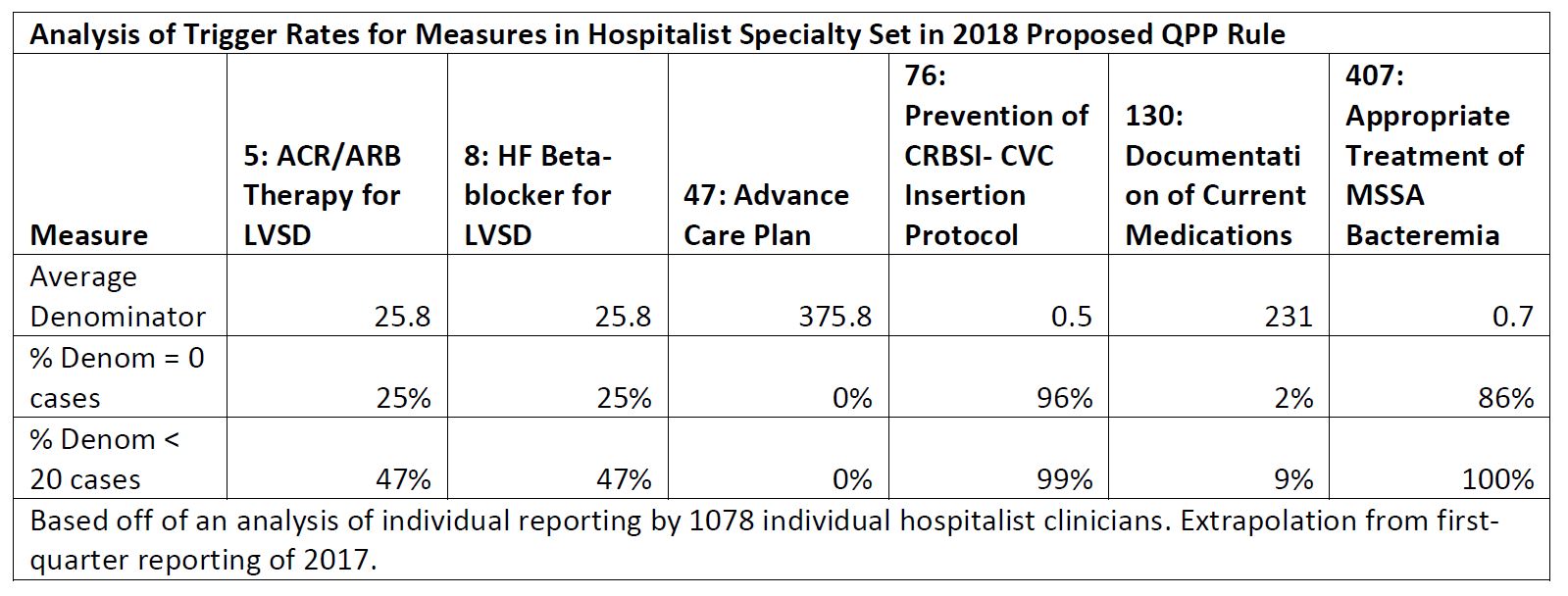
Of the measures available in the hospitalists specialty set, several are typically low-volume measures especially when providers choose to report at the individual level. For example, measures 76 and 407, when reported by hospitalists, rarely meet the measure volume threshold (20 cases) to be scored. Measures that do not meet the case minimum would receive three out of ten (3/10) points according to the proposed scoring policies in II.C.7 of the proposed rule. Per SHM’s analysis of the table below, many hospitalists will ultimately receive 3 out of 10 points for at least two measures. As such, SHM has serious concerns that hospitalists reporting these low volume measures will inadvertently set themselves up for lower scores and put themselves at inherent disadvantage. This is not an acceptable outcome and we strongly urge CMS to develop a solution for providers with low-volume measures, such as removing low-volume measures from the Quality category score.
II.C.6.b.(3)(b) Data Completeness Criteria
CMS proposes to keep the data completeness criteria for quality measures in 2018 reporting at 50% of Medicare Part B patients seen during the performance period and also proposes to raise the data completeness criteria to 60% for performance year 2019/MIPS payment year 2021.
We support CMS’ proposal to maintain the data completeness criteria at 50% for 2018. Many providers are still learning the requirements for the MIPS and setting up the processes necessary for successful participation in the program. Hospitalist groups have conveyed difficulty in setting up their data collection processes, which has led to issues with data completeness in the past few years. We believe it is appropriate to give providers additional time to learn and make improvements to their reporting processes.
SHM further encourages CMS to wait on increasing the data completeness criteria until after the first year of performance data from the MIPS program becomes available. This would enable CMS to analyze the impact increased data completeness criteria may have on provider performance. If it becomes apparent that providers are still struggling with data completeness, we caution against moving forward with any increased data completeness requirements.
II.C.6.c.(2) Topped Out Measures
CMS proposes a cycle to remove topped out measures from the MIPS measure inventory. The cycle follows a four-year process, in which a topped out measure is identified in the benchmarks, published in rulemaking as topped out, and finally removed from the program. SHM has consistently supported a transparent process for removing topped out measures from its programs. We encourage CMS to finalize this proposal to remove topped out measures in a structured manner, as it provides both notice and time to develop or identify replacement measures.
II.C.6.d.(2) Cost Performance Category Weighting in Final Score
CMS proposes to reweight the Cost category score to 0% for the 2018 performance/2020 payment years of the MIPS program, continuing the current transition year policy. SHM supports this proposal and we encourage CMS to work with Congress to modify the statutory requirement of 30% cost category weight by 2019. This modification could allow for a more moderate scaling up to 30%, for example 10% in 2019, 20% in 2020 and 30% in 2021. We support CMS including the details of physician/physician group performance on applicable cost measures (e.g., MSBP and Total Per Capita Costs) and providing details regarding patient attribution in the 2017 and 2018 feedback reports (to be released in 2018 and 2019 years respectively). There is a significant amount of confusion around the attribution methodologies of cost measures and including these details in feedback reports, even for the performance years when the measures are not scored, will help providers begin to understand their relationship to the measures.
II.C.6.d.(3)(iii) Episode-based Measures
CMS proposes to remove the previously finalized 10 episode-based cost measures from the Cost category. They note that they are currently in the process of developing new episode-based cost measures with more stakeholder input. As partners with CMS in efforts to develop these new measures, we support this proposal.
II.C.6.e.(3) Improvement Activities Data Submission Criteria
CMS seeks comment on whether they should establish a threshold of providers in a group to complete an improvement activity for the group to receive credit on the activity. For instance, CMS could require 50% of the NPIs within a group to complete the activity to assign credit.
SHM does not believe CMS should create a threshold for determining whether a group should receive credit for performing an activity. Some activities may naturally enable this sort of assessment, such as identifying those clinicians who have signed up and are using a state’s Prescription Drug Monitoring Program (PDMP). However, other activities may make less measurable, but still valuable, changes to provider practice. Many Improvement Activities require changes to provider workflow, which inherently affects most or all of the providers in a group. However, measuring how many of those providers complete a given activity may be difficult and require manual assessments. Adding a threshold to the Improvement Activities category would add unnecessary reporting burden to the program and would not yield meaningful feedback to CMS or providers.
II.C.7.a.(4) Facility-Based Measures Scoring Option for the 2020 MIPS Payment Year for the Quality and Cost Performance Categories
SHM has consistently advocated for and supported the development of an option for facility-based providers to align their performance with their facilities. We applaud CMS for proposing to turn this concept into a reality. We strongly believe the establishment of this option is rooted in a team-based approach to quality improvement and the reduction of administrative burden. Many hospitalists are already focused on and often incentivized to help their facilities meet performance on a range of metrics in multiple facility-level programs. These include the Hospital Value-Based Purchasing (HVBP), the Hospital Readmissions Reduction Program, the Hospital-Acquired Conditions Reduction Program, and the Inpatient Quality Reporting Programs, in addition to achieving and maintaining Joint Commission accreditation. The goals of these facility level programs and their attendant measures are broadly the same goals of the hospitalist providers who work in these settings. Hospitalists are, by nature of their practices, team-based and systems-oriented providers for whom the measures within PQRI, PQRS and now the QPP, have made very little sense. As a reporting option, facility-alignment will enable greater harmony between the performance of providers and their facilities while virtually eliminating the duplicative reporting burdens associated with provider-level quality measurement.
CMS proposes to convert facility scores from the HVBP Program into a MIPS score for the Quality and Cost categories. Specifically, they propose to use the hospital’s FY 2019 HVBP Program year. To be transparent and enable informed decision making about the facility-based measurement option, CMS also proposes to notify providers about their hospital’s performance in HVBP prior to election or application of the option. SHM supports both proposals.
We believe providing maximum transparency for providers about their reporting options will help to alleviate confusion and minimize administrative burden. While we acknowledge this approach may, at face value, appear to disadvantage non-facility-based MIPS eligible clinicians, it also comes with risks that are not borne by providers participating in the traditional MIPS. The HVBP Program in total contains measures that have varying degrees of applicability to hospital-based providers and that cannot be individually elected for reporting. Furthermore, individual providers do not have the same amount of control over performance via HVBP as they would with provider-level metrics in the MIPS.
CMS has chosen to launch the facility based option using the HVBP program in alignment with hospital-based providers. The central reason provided for this being that HVBP is the most mature of the facility measurement programs. SHM agrees with this assessment. However, CMS has indicated that this option could become available to providers within other facilities in future years. We urge CMS to continue to look at other facilities when expanding this program. Providers who are caring for patients within other facility settings often face similar obstacles with physician level reporting as hospitalists face in the
hospital setting. Quite often, hospitalists also provide care in SNFs or other post-acute settings and we encourage CMS to look to these facilities and their providers as a next step in facility alignment efforts.
Facility-Based Measurement Applicability
CMS proposes to consider an eligible clinician facility-based if they meet a threshold of 75% or more of their covered professional services in Place of Service (POS) codes 21 (inpatient hospital) or 23 (emergency room). This is a narrower definition than the MIPS Advancing Care Information hospital-based threshold, which includes POS 22 in addition to 21 and 23.
We strongly urge CMS to more closely align the eligibility threshold for facility-based measurement with the ACI definition of hospital-based by incorporating observation services delivered in POS 22. Observation services are virtually indistinguishable from inpatient care and frequently occur on the same wards of the hospital. CMS cites the time-based limitations for observation services (the ‘two-midnight rule’) as mitigating the effects of observation care on meeting the threshold. We disagree with this interpretation. While it is true observation is generally time-limited for a given patient, practice structures and provider scheduling have a profound effect on the proportion of observation care an individual clinician provides. Hospitalists who are on observation service, for example, may have a very high proportion of observation (outpatient) billing. This could exclude many hospitalists from qualifying for the facility-based reporting option, despite the fact they are truly hospital-based inpatient providers. It is not unusual for some hospitalists to see 20-30% of their patients under observation status. Despite the differences observation represents as a billing/payment distinction, observation care is a pervasive aspect of providing inpatient hospital care and must be accounted for in eligibility for facility-based measurement.
If POS 22/Observation cannot be fully included in the 75% threshold calculation, CMS should consider the following alternatives:
- Include POS 22 and couple the calculation with a cross-check to ensure most other billing is also hospital-based (POS 21 & POS 23). As a further check, CMS could look at specialty codes – is the provider also enrolled in Medicare as a Hospitalist (C6)?
- At a minimum, CMS could consider lowering the 75% threshold to 70% or, ideally, 60%. Due to the wide variation in hospitalist practice, we are uncomfortable with the use of thresholds in general, but lowering this threshold would at least provide a kind of safety net for hospitalists who are caring for high numbers of patients on observation.
Facility-Based Measurement Group Participation
CMS proposes to identify a facility-based group as eligible if 75% or more of their MIPS eligible clinician NPIs under the group’s Taxpayer Identification Number (TIN) are eligible for the facility based option. Alternatively, CMS considered whether a group could be deemed facility-based if they provide 75% or more of their covered professional services fall under POS 21 and 23. Due to high variability of group structure, billing patterns, and a lack of informative data, it is not possible to determine what method would work best for the majority of hospitalist groups at this time. Therefore, if administratively feasible, we recommend CMS determine eligibility using both proposed methods and, if a group qualifies through either, they should be deemed eligible for facility-based measurement.
This concept has precedent in CMS’ methodology for determining qualified provider thresholds under the Advanced APM pathway. CMS has decided to make QPP determinations by calculating both the patient and payment approach and using the option most favorable to the provider. We feel that a similar process for determining group eligibility for facility based scoring would enable the most groups to be eligible for this option.
Facility Attribution for Facility-Based Measurement
CMS proposes to give clinicians under the facility-based measurement option a score derived from the HVBP score at the facility in which they provided services for the most Medicare beneficiaries during the two years preceding the performance period. We understand CMS’ rationale for wanting to ensure a provider has a meaningful relationship with a given facility, and also the desire to minimize provider confusion with multiple scores. We support this methodology but, as CMS acknowledges, many providers practice in multiple facilities. We encourage CMS to work with stakeholders to develop a methodology to account for this reality in the future.
We also note the attribution proposal only considers individual facility attribution and does not account for groups under this option. Large groups can provide clinical care at a number of geographically discrete facilities, with some TINs containing as many as 30 facilities. If the attribution methodology is finalized as proposed for a group practice, and the sole facility where the plurality of Medicare beneficiaries was cared for becomes the attributed facility, then it is likely that a large group as identified by their TIN would have a Hospital VBP Total Performance Score attributed to that group for a facility where the group cared for only a small portion of their total Medicare beneficiaries. We encourage CMS to develop a methodology, either this year or in future years to account for groups practicing in multiple sites. This could be done by setting a threshold of services or patients, or through some form of an attestation process. Scoring for groups or individuals practicing in multiple sites could be achieved through a weighted average of the percentiles from those attributed hospitals.
Election of Facility-Based Measurement
CMS proposes to have an attestation process for eligible clinicians to elect the facility-based measurement option during the data submission period and has put forth an alternative proposal to automatically calculate the facility-based measurement score for all eligible providers. While we support the opt-in attestation and agree it is minimally burdensome, we prefer CMS’ alternative proposal to automatically calculate the facility-based measurement score for all eligible providers.
Consistent with a desire to decrease the burden for eligible clinicians and group practices in MIPS, we believe it is most appropriate to automatically assign the best achievable score (either a Hospital VBP score or a MIPS score) to those clinicians deemed to be facility-based. It is unreasonable to assume that clinicians would opt to choose a less advantageous score if both were available. Therefore, an “opt-in” process (when the most advantageous score can be chosen) is a redundant step, and could risk confusing and possibly penalizing those who fail to understand all the nuances of the program.
Assigning MIPS Performance Category Scores based on Hospital VBP Performance
Providers who are eligible for the facility-based measurement option would receive scores in the Quality and Cost categories based on their facility’s performance in the HVBP. The clinician would be given the same percentile score in each MIPS category as the percentile the hospital scored in the HVBP Program.
We support this proposal as it is a clear and easy to understand mechanism for translating a facility score into a provider-level program. Using the percentile accounts for the fact that the HVBP and the MIPS are not likely to have similar score distributions or performance thresholds and will allow for a smooth transition.
We do have some concerns about the impact of this policy on a provider scored under this option as the MIPS final score transitions from a CMS-set performance threshold to the mean or median of performance in the MIPS. We ask CMS for more detailed modeling about how this shift in the overall program scoring may affect providers who are participating in the facility-based measurement option. We also ask CMS to remain open to addressing any issues or inconsistencies that may arise as the program continues to mature. This concern is particularly germane given our support for CMS’ proposal to automatically calculate scores for the facility-based reporting option. We do not view providers simultaneously reporting the traditional MIPS and being scored under the facility-based measurement option as a tenable long-term strategy – they will ultimately commit to one or the other once a comfort level is achieved. Therefore, we ask CMS to provide as much information about the MIPS performance threshold and how it would affect scoring under facility-based measurement as early as possible.
Bonus Points for Facility-Based Measurement
CMS does not propose any bonus points for providers who elect facility-based measurement, by noting the Quality and Cost categories percentile distributions would contain any bonus points that could be gained by providers reporting the MIPS measures.
We disagree with CMS’ assertion that bonus points built into the percentile distribution accurately account for the bonus points awarded to outcome and other high-priority measures. As CMS acknowledges, many of the measures in the HVBP Program would be considered high-priority measures in the MIPS. As one alternative, CMS could develop a complex patient bonus for clinicians who opt for the facility-based measurement option. Specialties like hospitalists see sicker patients with more complex health issues than many of their outpatient counterparts, and so we urge CMS to give a complex patient bonus to providers who elect facility-based measurement. We do not believe the VBP program adequately adjusts for patient complexity and we want to ensure our physicians are still eligible for a comparable bonus. This approach would look similar to the complex patient bonus for MIPS eligible clinicians generally, but account for the severity of patients seen by the facility.
Particularly if CMS finalizes an opt-in for the facility-based measurement option, we urge CMS to develop a bonus to encourage participation in this option and as an acknowledgement of the tradeoffs associated with the option. Facility-based measurement is a significant philosophical shift in the relationship between facilities and providers and refocuses both on achieving the same goals. The option also creates an incentive for both parties to pursue additional quality and process improvement efforts that would lead to improvement on hospital metrics and, ultimately, improve patient care and outcomes. At the same time, individual providers will have less direct control over their performance and score under this option when compared against traditional MIPS reporting. We are concerned that in the absence of any bonus points or incentives, those providers who work in hospitals that may not perform well under HVBP will avoid electing this option. We see a strong potential for performance improvement in lower performing facilities when the providers and facilities share the same measure goals and we do not want this alignment to be limited to only providers in high-performing facilities.
Special Rules for Facility-Based Measurement
CMS proposes to create a performance floor of 30% in the Quality category for providers who elect the facility-based measurement option. We urge CMS to finalize this proposal as it is equivalent to the 3-point floor for measures in the Quality category of the MIPS. Since a MIPS eligible clinician can report on 6 measures and receive 3 points for each measure regardless of performance, any lower performance floor would disadvantage providers who select the facility-based measurement option.
SHM also strongly supports the option for scoring both MIPS and HVBP, and taking the higher score for those clinicians or groups who qualify for the facility-based measurement option and report normally under the MIPS. The facility-based measurement option is different from reporting MIPS measures and requires clinicians to give up a significant amount of control over selection of measures and their performance. Scoring both would allow groups who are uncertain about the facility-based measurement option to “test” the option while maintaining control over their MIPS performance by reporting on quality measures.
II.C.7.b.(3)(d) Redistributing Performance Category Weights
SHM supports CMS’ alternative approach for redistributing the weight of the Advancing Care Information category to both the Quality and the Improvement Activities categories. While it is true that providers have the most experience with quality measures and we recognize that Improvement Activities is a relatively new category, we strongly oppose a hospitalist’s payments being based 85% on their performance on quality measures.
In addition, we believe Improvement Activities have the potential to be more transformative and impactful at the local level. Reweighting towards this category would encourage additional attention and resources for these activities. It is the least static category, with more opportunities for providers to engage in quality improvement activities relevant to their practice and to address clinical realties. Providers can more readily identify localized gaps and execute local-level performance improvement efforts to address those gaps than they can engage in the development and shepherding of new quality measures, which is a complex, time-consuming, and costly endeavor.
II.C.8. MIPS Payment Adjustments
CMS has previously finalized policies to have the MIPS payment adjustment follow unique Tax TIN/NPI combinations, or in cases where a provider changes TINs, at the NPI level. Functionally, this means that a payment adjustment will follow an individual provider regardless of where they are practicing during the payment year of the program. We have concerns about this policy and its unintended consequences for individual clinicians and their employers.
Group practices make substantial investments to comply with overall MIPS goals, specifically to monitor, educate and train physicians in quality behaviors and to capture quality data for reporting to CMS. These investments are made to ensure providers within a given group are able to participate in the program. However, many group practices are not made up of a static group of clinicians; it is not uncommon for a company to have around 20% turnover in a given year. Given the lag between the performance and the payment years, somewhere between 20 and 40% of a group may turnover. This means a significant amount of payment adjustments (both positive or negative) are constantly in flux and the resultant revenue for the group is uncertain. This creates serious risks for stability in group finances, while simultaneously disincentivizing investment in the MIPS goals.
Individual clinicians may also face barriers in employment as a result of payment adjustments applied to their Medicare Part B billing. Individual providers do not always have control over whether their group decides to report under the MIPS. Furthermore, the measures, and therefore the payment adjustments, may not actually reveal whether a provider is low-quality. Given the serious concerns with the fidelity of quality data and the attribution of providers to patients, SHM believes the current payment policies will disadvantage providers as they seek employment opportunities.
We strongly encourage CMS to work with stakeholders to develop a way for group practices (TINs) to retain 100% of the financial accountability for their MIPS performance. This could be achieved by creating a group-level attestation with a lump sum payment/recoupment as part of the payment. It could also be achieved by developing processes to make payment adjustments as close to real time as possible.
II.C.8.c. Establishing the Performance Threshold
CMS proposes to set the performance threshold for the 2020 MIPS payment year at 15 points. Further, they indicate the statute requires them to set the performance threshold for the 2021 MIPS payment year at either the mean or median final score from a prior year. As CMS discusses, this could lead to a performance cliff in the transition between 2020 and 2021 payment years. While we support the lower performance threshold of 15 as another aspect of CMS’ efforts to ease the transition into the new program, we share the concerns that the shift to mean or median could lead to significant confusion and disruption. We urge CMS to share their analyses and modeling as they collect more data and indicate to stakeholders their expectations for how this transition will impact performance as early as possible. We also encourage CMS to be mindful of this performance threshold gap as they promulgate future rules and look for ways to mitigate significant issues.
Alternative Payment Model (APM) Incentive
SHM fully supports the intent of the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 to move away from fee-for-service payment in healthcare and incentivize the adoption of alternative payment models (APMs). After reviewing the proposals for the APM Incentive, SHM remains concerned that many providers will be unable to access the QPP incentive for Advanced APM participation given the continued lack of available Advanced APMs. We also remain extremely skeptical of the ability for providers to meet the increasing thresholds associated with the incentive.
Our concerns are particularly salient for provider-driven models. Hospitalists’ experiences with the Bundled Payments for Care Improvement (BPCI) model highlights the difficulty providers will face in meeting thresholds for Qualifying Participant (QP) status. Provider-driven models tend to be smaller in scale and episode or condition specific. As such, they capture only a portion of a provider’s patient population, inherently limiting the number of patients or payments attributable to the numerator of the QP determination.
None of the proposed policies, including the groundwork for the all-payer options, address these fundamental barriers to successful QP determinations. Given the stated goals of the APM incentive to foster new APMs and greater participation in those models that move farther away from traditional fee-for-service, we believe CMS needs to use its authority to its fullest extent to make the APM incentive pathway more accessible. We also note that there may be statutory changes necessary to meet this goal and urge CMS to begin working now with Congress and other stakeholders to address any statutory changes that may be needed.
All-Payer Combination Option
CMS rightfully recognizes that there may be medical homes that are operated by other payers that may be appropriately considered medical home models under the All-Payer Combination Option and seeks comment on the characteristics used to determine an ‘Other Payer Medical Home Model” as an other payer arrangement. Although SHM is not commenting on the usefulness or validity of the proposed characteristics, should these characteristics be finalized, SHM does have comments on the “Primary Care Focus” characteristics. Under this set of characteristics, CMS defines primary care focus to mean inclusion of specific design elements related to eligible clinicians practicing under one or more of the following Physician specialty codes: 01 General Practice; 08 Family Medicine; 11 Internal Medicine; 16 Obstetrics and Gynecology; 37 Pediatric Medicine; 38 Geriatric Medicine; 50 Nurse Practitioner; 89 Clinical Nurse Specialist; and 97 Physician Assistant. As a primary care specialty, many hospitalists work directly with primary care practices in providing inpatient primary care to that practice’s patients. As such, SHM recommends the addition of C6 Hospitalist to this list of characteristics.
Medicare Health Plans – Medicare Advantage for QP determinations
SHM fully supports creating a path whereby current and future APM participants can have their participation in Medicare Advantage plans count towards their eligibility as a QP under the Medicare advanced APM option. To qualify for the five percent advanced APM bonus, APMs must have a certain threshold of their Part B revenue or patients in the advanced APM. For the first two years of MACRA implementation, that threshold includes 25 percent of Part B payments or 20 percent of Part B patients. In later years, the Medicare Part B threshold increases to 50 percent and then to 75 percent. As indicated previously, SHM has serious concerns about provider’s ability to meet these thresholds as participants in the models currently available. The ability to include Medicare Advantage participation toward meeting threshold goals would be welcome relief for groups who have invested heavily in APM participation (including Medicare Advantage) and yet may not meet QP Thresholds.
Conclusion
SHM appreciates that CMS has spent a significant amount of time talking to and working with providers on developing the second year policies for the Quality Payment Program. We strongly urge the agency to continue this high level of engagement as it continues to develop and refine the QPP. We remind CMS that as an evolving program, the QPP may need additional changes and corrections to mitigate unintended consequences and issues that may arise. SHM stands ready to work with CMS on implementing and future policies for the QPP to ensure that the nation gets a higher quality, more efficient healthcare system.
Sincerely,
Ron Greeno, MD, FCCP, MHM
President, Society of Hospital Medicine
